Is PAO Surgery the Right Choice for Your Child?
 By Shane Dowd, CES, CMP
By Shane Dowd, CES, CMP
Is PAO Surgery the Right Choice for Your Child?
Imagine this: Your kid’s got hip pain, so you visit the local doctor. After doing some exams, you find out your kid has hip dysplasia, and it’s (theoretically) causing all their hip pain…
The doctor says that one of the treatments is a surgery called Periacetabular Osteotomy or PAO.
That night, you frantically search the Internet to figure out “what the hell is PAO” and whether it’s a good idea.
In this video, we will explore:
-
What is PAO Surgery? Does it work?
-
How long it lasts
-
What your other options are
What is Hip Periacetabular Osteotomy?
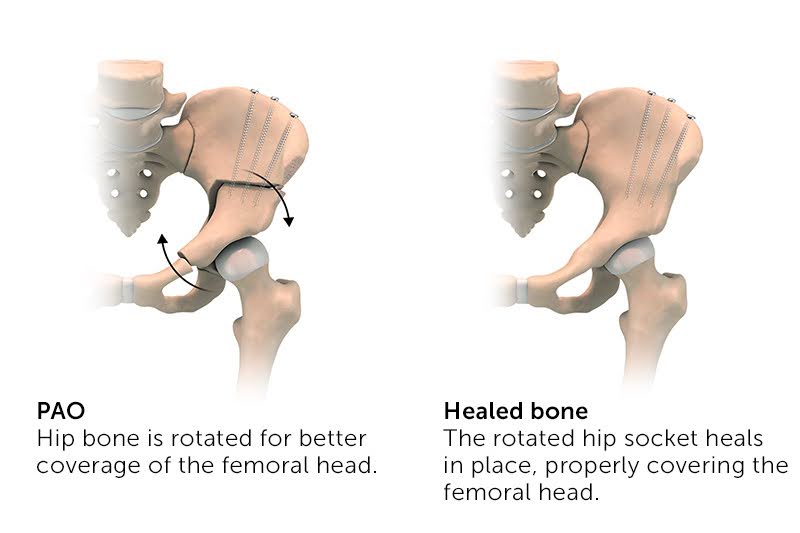
Periacetabular Osteotomy, AKA PAO surgery, means that a surgeon will cut and detach one half of the pelvis and rotate the hip socket downward. Theoretically, this intensive procedure is used to treat a shallow socket (hip dysplasia).
The theory is that the patient is born with a shallow hip socket and that this may cause hip arthritis at a young age.
Hence, Hip PAO surgery is supposed to cover the unprotected part of the hip to reduce the need for an early hip replacement.
While all of this sounds…sorta…kinda reasonable, let’s explore how much science knows about this procedure.
How Long Does Hip PAO Last? (Not Long Enough…)
The first and most critical question to ask is: how long does it last?
10 years? 20 years? A lifetime?
After all, if you’re going to have half of your pelvis completely disconnected and then reconnected, is this a one-time thing? If not, how much additional time will you have before you need that hip replacement?
A recent large meta-analysis of several hip PAO scientific studies that
- 75.9% of patients avoided hip replacement at 10 years
- 36.5% of patients avoided hip replacement at 20 years
In plain English, this means:
- We have a crazy invasive surgery used in young patients
- This surgery is intended to replace or delay a hip replacement
- But 1 in 4 patients who get the PAO procedure still end up needing a hip replacement after only 10 years
- And 2 in 3 still need a hip replacement at 20 years?
I don’t know about you, but I wouldn’t like those odds for me OR my kid.
The Big Mystery: Does PAO Surgery Work? Who Knows?!
The medical “Gold Standard” for determining whether a treatment works is a randomized controlled trial (RCT). In an RCT, you compare the treatment to something else or a placebo.
In other words, one group of patients gets the treatment you’re testing and the other group gets a different but standard treatment (like physical therapy or a placebo or sham procedure).
So, what does the RCT data say about whether PAO works?
Unfortunately, the answer to that is… who knows?!
At the moment, there is a lack of RCTs, the “gold standard” evidence. The scary thing (for you or your kid) is that there is very little high-level evidence that this invasive surgery saves patients from a hip replacement.
That’s critical because you would expect at least a few long-term studies looking at patients who got hip PAO surgery versus those who didn’t.
That would be the only way that you could convincingly say that the surgery helps to reduce the need for a hip replacement.
While some studies are in progress, most of them are still in the category of “low-level evidence”.
What does this mean for you?
Be careful before rushing into a surgery before exhausting all other nonsurgical options. This is an important decision. Especially if it means subjecting yourself or your child to an endless chain of future surgeries.
Complications of Hip PAO Surgery (What Else Could Go Wrong?)
If you’re considering a PAO surgery, and have maxed out all nonsurgical options, it’s important to go into it with eyes wide open.
A 2021 meta-analysis of almost five thousand patients represented by 33 articles showed that the mean hip PAO complication rate was 14.1% or about 1 in 7 patients.
That puts hip PAO in the high-risk orthopedic category. For example, the complication rate of knee arthroscopy surgery is about 1%.
Common complications of this surgery include:
- Nerve Damage: Risk of harming nerves near the hip.
- Blood Loss: Significant bleeding during the operation.
- Infection: Possible infection at the surgical site.
- Bone Healing Issues: Bones may not heal properly or align well.
- Heterotopic Ossification: Abnormal bone growth in surrounding soft tissue.
- Pain and Stiffness: Ongoing discomfort and limited movement in the hip.
- Blood Clots: Potential for dangerous clots forming in veins.
- Limited Mobility: Reduced range of motion in the hip.
- Additional Surgeries: Possibility of needing more operations if problems arise.
The Future of Hip Dysplasia Treatment
The concept behind hip PAO surgery is to “catch it early” and reduce the need for hip replacement surgery in your 40s to 50s.
But, why does hip arthritis occur at these ages?
Basically, because “wear and tear” can no longer keep up with “wear and repair”.
Theoretically, you can reduce the wear and tear with surgery like PAO.
But, as I cover in THIS video about hip arthritis, you aren’t doomed. Hip arthritis CAN be managed, improved, and even healed!
You don’t have to be a passive victim and you CAN improve your abilities to “wear and repair” as you age.
How? Mindful, intelligent, strength, and stability training.
The Bottom Line: What Should You Do?
This is a tough choice for any parent or child…
Do you get a very invasive surgery to section the pelvis and re-attach it? Do you hope that you’re in the 1 in 3 that gets at least 20 years more time before needing a hip replacement?
If the RCT science said that hip PAO worked dramatically better than doing nothing or working on it mindfully, THEN, maybe it would be worth the risk.
But, that research just ain’t there yet.
My Personal Opinion As a Former Hip Pain Sufferer:
So what do I think? What’s my opinion as someone who was also told at age 26: “Don’t be an idiot, go get hip surgery!”
For me, I am not impressed with the results of hip PAO surgery compared with the risks.
Is it possible that new research will change everything? Maybe. But so far, the research into this surgery is of poor quality, given the massive risk to the patient.
Ultimately, I always prefer less invasive, less expensive options. That’s why, for the past 14+ years, since recovering from my own hip problems, I’ve dedicated my life to helping others heal – without surgery.
If you want to see how we’ve helped over 30,000 people get better with our TSR Method, check out our “do it yourself” hip pain program at the link in the description.
Or, if you’re looking for a higher level of support, go to gotrom.com/vip to apply for our Hip Fix 1:1 Coaching Program.
I hope this video was insightful, and, as always, please remember – you’re just 1 step away from building (or rebuilding) your perfect body.
________________________________________________
References:
(1) Coobs BR, Xiong A, Clohisy JC. Contemporary Concepts in the Young Adult Hip Patient: Periacetabular Osteotomy for Hip Dysplasia. J Arthroplasty. 2015 Jul;30(7):1105-8. doi: 10.1016/j.arth.2015.02.045. Epub 2015 Mar 25. PMID: 25865812.
(2) Gala, Luca MD1; Clohisy, John C. MD2; Beaulé, Paul E. MD, FRCSC1,a. Hip Dysplasia in the Young Adult. The Journal of Bone and Joint Surgery: January 6, 2016 – Volume 98 – Issue 1 – p 63-73 doi: 10.2106/JBJS.O.00109
(3) Tan JHI, Tan SHS, Rajoo MS, Lim AKS, Hui JH. Hip survivorship following the Bernese periacetabular osteotomy for the treatment of acetabular dysplasia: A systematic review and meta-analysis. Orthop Traumatol Surg Res. 2022 Jun;108(4):103283. doi: 10.1016/j.otsr.2022.103283. Epub 2022 Apr 22. PMID: 35470119.
(4) Beck EC, Gowd AK, Paul K, Chahla J, Marquez-Lara AJ, Rasio J, Irie T, Williams J, Nho SJ. Pelvic osteotomies for acetabular dysplasia: Are there outcomes, survivorship and complication differences between different osteotomy techniques? J Hip Preserv Surg. 2021 Feb 5;7(4):764-776. doi: 10.1093/jhps/hnab009. PMID: 34377519; PMCID: PMC8349594.
(5) Parilla FW, Ince DC, Pashos GE, Maloney WJ, Clohisy JC. Long-Term Follow-Up of Conventional Polyethylene in Total Hip Arthroplasty in Young Patients: Heightened Wear-Related Complications Are Observed at the Beginning of the Third Decade. J Arthroplasty. 2022 Sep;37(9):1816-1821. doi: 10.1016/j.arth.2022.04.011. Epub 2022 Apr 21. PMID: 35460812.
(6) Friberger Pajalic, K., Turkiewicz, A. & Englund, M. Update on the risks of complications after knee arthroscopy. BMC Musculoskelet Disord 19, 179 (2018). https://doi.org/10.1186/s12891-018-2102-y
About The Author











